Your Voice on COVID-19: Sumter native is a traveling nurse in NYC
Community contributor
We've been asking our Sumter Item community to share their stories surrounding COVID-19 and the pandemic's impact on you, your family and friends, work, etc. We want to tell the stories of the people in our community, putting names and people to statistics and trend articles.
To share your story and read other submissions, go to https://bit.ly/3e3kcvf or email editor@theitem.com if you want us to send you a questionnaire. You can also call (803) 774-1235 and leave a voicemail either detailing your story or a callback number.
* Editor's note: While we read through and edit these reader submissions to ensure they adhere to our publishing policy, we cannot fact-check all of these personal experiences. The Sumter Item does not endorse opinions that may appear in Your Voice.
---
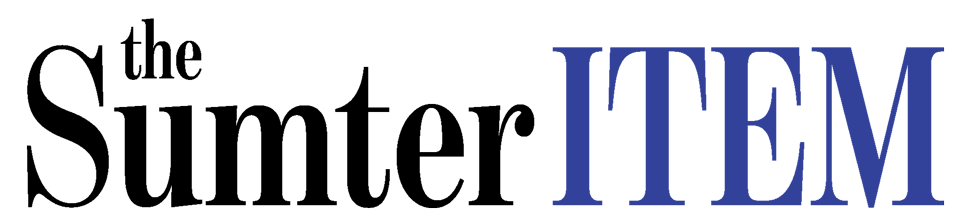
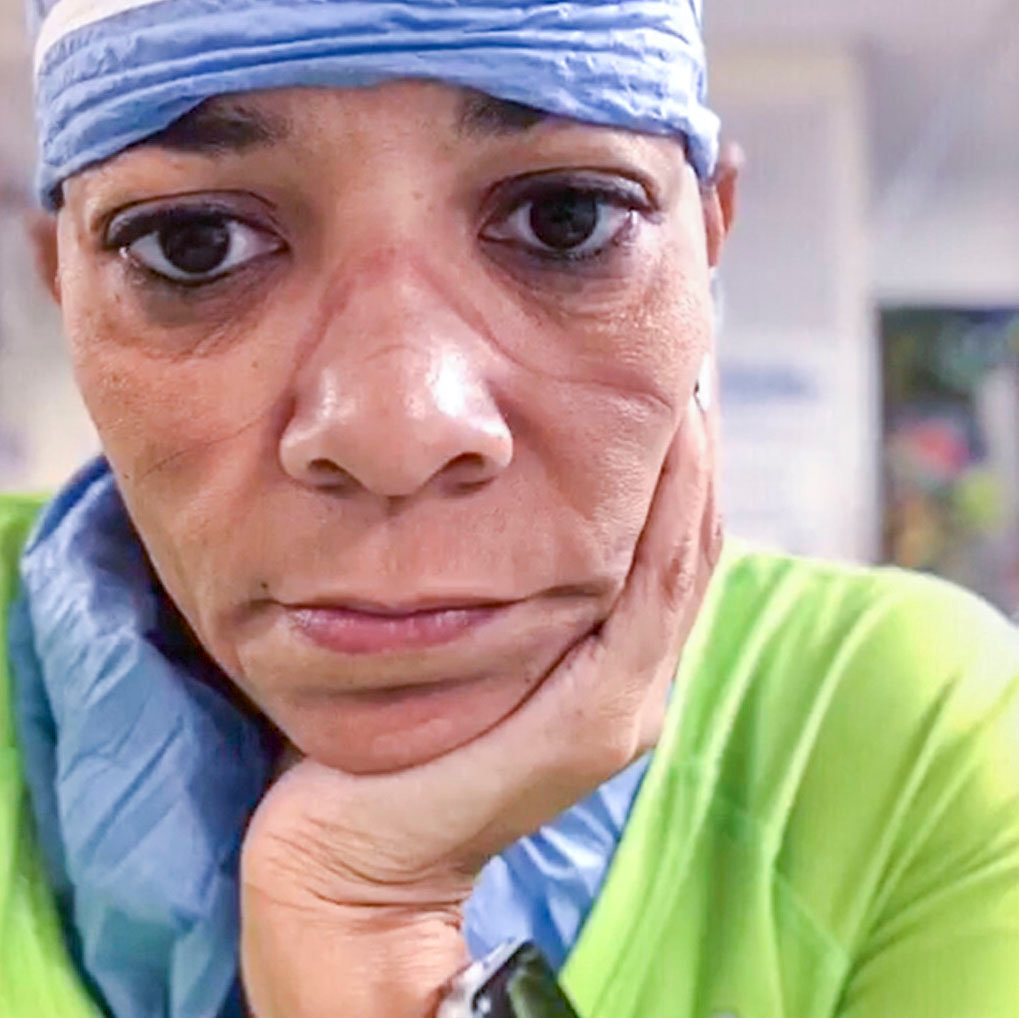
Latasha Stevens is currently working at Harlem Hospital Center in New York City as a registered travel nurse to help people fight COVID-19 in one of the nation's hardest-hit cities.
The 47-year-old said she is a 1991 Hillcrest High School graduate and that her mother still lives in Sumter. They try to Skype daily.
Her work schedule is intense and seemingly incessant, meaning sitting down for a phone interview would be difficult to arrange, so she wrote to The Sumter Item through its Your Voice platform to share her story.
---
I am a registered travel nurse. I was working as a travel nurse in North Carolina working at a psychiatric hospital when I got the opportunity to deploy to New York. It was a Sunday when I got the call, and they wanted me to be in New York within 24 hours because of the desperate need for help. I remember when I was packing my things, my hands were shaking, and my mind was all over the place. I prayed to God to "order my steps," but I made my ultimate decision when I asked myself, "What would my late Daddy (Kal Stevens Jr.) want me to do?" With that question answered in my head, I took a deep breath, finished packing my things and went to the airport in Raleigh, North Carolina.
Arriving, I was so petrified, and I remember thinking, "What are you doing, big dummy?" I checked in and got on the plane headed to LaGuardia.
My first day heading into work was emotional but powerful to see New Yorkers come together with cheers, honks and claps to reassure us that we were appreciated and to thank us for coming to help keep the city alive. I got assigned to Harlem Hospital, and when we got there, its patient population was 100% COVID-positive. They had only about 19 New York staff nurses in the entire hospital still working (the others had either quit or had gotten sick). We brought about 160 travel nurses with us, and when we got to the auditorium on our first day, I remember overhearing one of the New York nurses nudge and whisper to her coworker, "The cavalry has arrived."
When we got to the units, I vividly remember seeing patients who are critically sick, alone and had panic in their eyes. I don't care how long I live, I will never forget the look that was in their eyes. It was universal from patient to patient, and it gave me a feeling of anxiety that I cannot describe. The patients were scared, and so were we. It truly got real for me when we started to don our PPE. My hands shook, and I would hyperventilate every time! The gowns and scrub caps and gloves and masks and googles were overwhelming and sooooo HOT but so very necessary. We wore so much gear 100% of the time while at the hospital, which was exhausting in itself. My nursing skills were challenged over and over again, but imagine trying to insert an IV into a critically ill patient whose veins are nonexistent due to dehydration. Imagine sweat dripping from places you didn't know you had inside all that PPE. Now imagine your face shield and glasses are fogged up from heavy breathing and nervousness, making it difficult to see. Lastly, imagine that the patient is COVID-positive. He is coughing uncontrollably, putting lung secretions all over you, AND his life is depending on you to place the IV NOW!!! Talk about pressure.
I was raised in St. Paul AME Church on Plowden Mill Road in Sumter all my life, literally. This church, its pastors, the Rev. Fred Graves and Sidney Hampton, and its members gave me unwavering support during my time in New York. Growing up in Sumter, my mom, Rita (Jo Jo) Stevens, made sure we went to church, and she made sure we knew God and we knew the Word of God. I have been taught to trust him and to pray daily. I prayed all day sometimes while in New York, but I never questioned or second-guessed the reason I was now a COVID-19 nurse and working in a 100% COVID-unit. As we say in my culture/community, "God makes no mistakes." My daily prayer as I walked into Harlem Hospital came from the book of Psalms 23: 3-4, and it reads: "He restoreth my soul; he leadeth me in the paths of righteousness for his name's sake. Yea, though I walk through the valley of the shadow of death, I will fear no evil: for thou art with me; thy rod and thy staf,f they comfort me ..."
Once on the unit, we quickly went about our business of treating patients, very, very critical patients. We worked many, many hours. We were weary and overwhelmed, but we kept coming into work and kept trying to save lives. We would work tirelessly through breaks and meals sometimes. We worked 12 hours a day, seven days a week, and every nurse was scared, tired and weary and pushed to their limits. There were so many sick patients ... way more than there were beds. Some were in the hallways begging for help. Some were on stretchers for days because there were no beds available. Sometimes, we had no idea who some patients were or what their names were, and they ended up dying with the name unknown, York.
Most units had very little or no supplies like insulin needles, gowns or much-needed rebreather masks. I remember we would improvise and stuff latex gloves in holes of an oximask to make it into a rebreather mask, and it worked wonders on patients who were hypoxic. I remember seeing patients on 15 liters of oxygen, and they would still crash and die from respiratory distress. Nearly every patient's code status was DNI/DNR, meaning do not intubate/do not resuscitate. Meaning no matter what happens, do not do CPR because we are not going to save this patient. Let that sink in for a minute. You will never "un-see" a person struggling to breathe, and you can do nothing but stand there and comfort them, hold their hand and watch them die. Patients died. Many died suddenly and helplessly, regardless of our efforts. Many times, more than I care to count, I remember a COVID-positive patient dying in a four-person room/bay, and the body would sit there in the bed, in the body bag for hours and hours while waiting on transport to come take it to the refrigerated trucks. Meanwhile, the other three patients were still in the room watching, COVID-positive also and mortified.
The outpouring of love and support from my community has been touching and overwhelming. My family and friends really showed their appreciation to these deployed COVID nurses here in NYC. I received boxes and boxes of goodies that I donated to the nurses nightly. Special thank yous to these organizations that sent boxes to us: The Mary McLeod Bethune section of The National Council of Negro Women, The South Carolina Retired Teachers Association, Jocelyn Bynum and Verizon. Many, many thanks to my Sumter/Dalzell/Hillcrest High friends and community, my Shaw University friends and family, WSSU classmates, friends and coworkers in North Carolina and Virginia. Lastly, my family has really held me up through this deployment. I love and appreciate all of you from the bottom of my heart.
I have been in New York for two months, and my time here is winding down. I have emotions that have I not processed or released because there is no place for that while on the frontlines working. I guess it will come with time, but at this time I do not have adequate words or descriptors. I will say, as an NYC COVID nurse, I was forced to step out of my nursing comfort zone while mentally and physically spent, and I will cope with the grief and despair now that my mind will have time to reflect and rest.
I answered the call as my dad did many years before me in Vietnam. Just as he described to me so many times before, I am proud to say I was there to help when I was needed, but the reality is that I am not a hero and do not want to be glorified as such. I am a nurse, and this journey is a major part of who I am. I didn't choose this fight. This fight chose me.